 Typically, in the UK, lacrimal dilation and irrigation are performed in hospital. However, with a little practice and care, it is a relatively simple
procedure for any optometrist or GP to carry out. The equipment required is inexpensive and easily obtained (see Appendices I and II).
This paper will review the relevant anatomy and physiology, discuss the aetiology and evaluation of epiphora (watery eye), and then explain
dilation, syringing and the various dye tests associated with investigating the lacrimal drainage system.
Typically, in the UK, lacrimal dilation and irrigation are performed in hospital. However, with a little practice and care, it is a relatively simple
procedure for any optometrist or GP to carry out. The equipment required is inexpensive and easily obtained (see Appendices I and II).
This paper will review the relevant anatomy and physiology, discuss the aetiology and evaluation of epiphora (watery eye), and then explain
dilation, syringing and the various dye tests associated with investigating the lacrimal drainage system.
|
 ANATOMY OF THE LACRIMAL
DRAINAGE SYSTEM
ANATOMY OF THE LACRIMAL
DRAINAGE SYSTEM
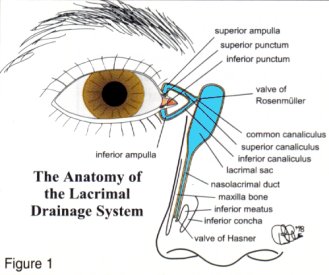
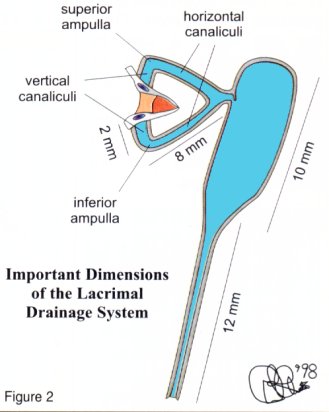
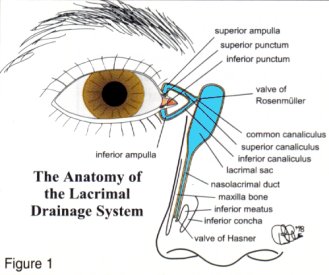
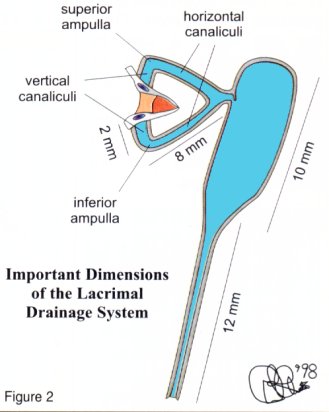
The anatomy of the complete
system is shown diagrammatically
in Figure 1. Some important
dimensions appear in Figure 2.
a) Puncta
One punctum is present at the
medial end of both the superior and
inferior lid. They are situated on
slight elevations called the lacrimal
papillae and face posteriorly so it is
necessary to evert the medial lids to
inspect them. Malposition or
stenosis (narrowing) of the puncta
may cause epiphora.
b) Vertical canaliculus
This is about 2mm long and joins the
horizontal canaliculus at a right
angle called the ampulla.
c) Horizontal canaliculus
This is about 8mm long and usually
joins its fellow to form the common
canaliculus which immediately
enters the (naso)lacrimal sac
through the Valve of Rosenmuller
(flap of mucosa to prevent reflux).
d) (Naso)lacrimal sac
This is about lOmm long and funnels
into the nasolacrimal duct.
|
|
e) Nasolacrimal duct
This is about l2mm long and opens
into the inferior nasal meatus, lateral
to the inferior turbinate (concha). The
Valve of Hasner closes the opening.
f) Valves
About seven other valves have been
described within the nasolacrimal duct
besides those of Rosenmuller and
Horner (see Last) but they have no
valvular function and are usually
ignored. |
PHYSIOLOGY OF THE LACRIMAL
DRAINAGE SYSTEM
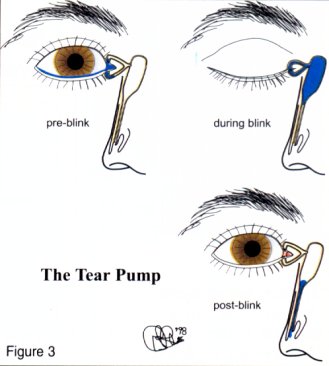
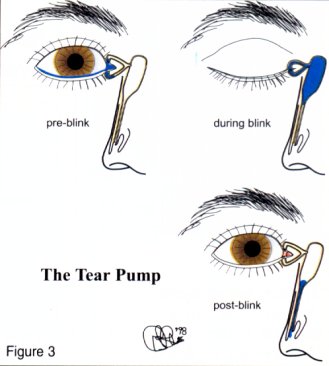
Capillarity ensures that 70% of the
tears enter the inferior canaliculus and
30% through the superior (Figure 3 -
pre -blink). On blinking, the
attachment of the preseptal orbicularis
muscle helps create positive and
negative pressure in the lacrimal sac
which sucks the tears into it (Figure 3
- during blink). This is called the tear
pump. Gravity then helps keep the sac
empty (Figure 3 - post-blink).
AETIOLOGY OF EPIPHORA
Epiphora may be due to a
hypersecretion of tears as occurs when
a foreign body irritates the cornea.
Paradoxically, it may also be due to an
underlying dry eye problem which, in
turn, causes a foreign body reaction
and tearing. Likewise, it may be due to
a lacrimal pump failure as in ectropion
when tears are no longer able to enter
the punctum. It may also be caused
by punctum plugs or punctum
cauterisation for the treatment of dry eye.
|
 |
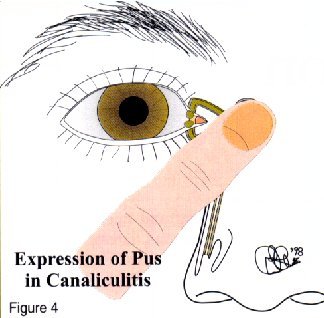
| EVALUATION OF EPIPHORA
a) General inspection
Inspect the lids to see if they and/or
the puncta are poorly positioned.
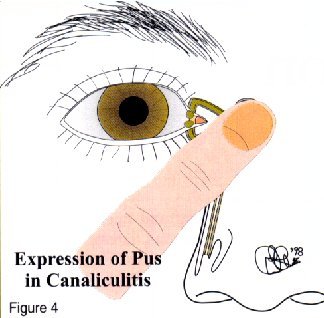
Palpate the lacrimal sac to determine if
it is enlarged due to dacryocystitis or a
mucocele. Compression may cause a
reflux of mucopurulent matter (Figure
4). Pain suggests dacryocystitis.
|  |
b) Slit lamp examination
Inspect the puncta for poor
position, narrowing or blockage
- pouting suggests canaliculitis.
A high marginal tear strip may
indicate epiphora. If fluorescein
is instilled in the conjunctival
sac, it should disappear within
two minutes - retention
suggests there is a problem with
lacrimal drainage. |
|
c) Irrigation
 |
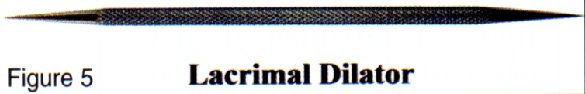
1) Lacrimal dilation
Several types of dilators are
available, for example the
double-ended stainless steel
type in Figure 5 ( see Appendix I) or those incorporated in
punctum plug inserters. Their
use may effect a cure by
releasing mucous plugs or
concretions. Dilation may
produce temporary relief in a
case of stenosis of the punctum.
Lacrimal dilation is also used
prior to inserting punctum
plugs and syringing.
- Wash your hands.
- Some practitioners may
wish to put on surgical
gloves.
- Instil a drop of anaesthetic
on the inferior punctum.
- Sterilise the lacrimal
dilator with a Medi-Swab.
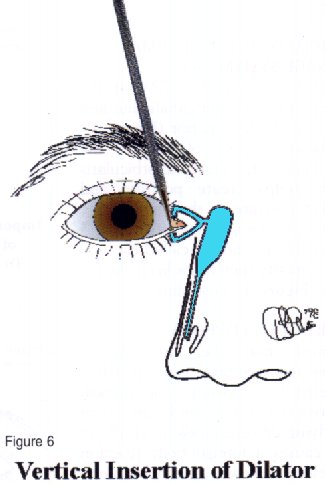
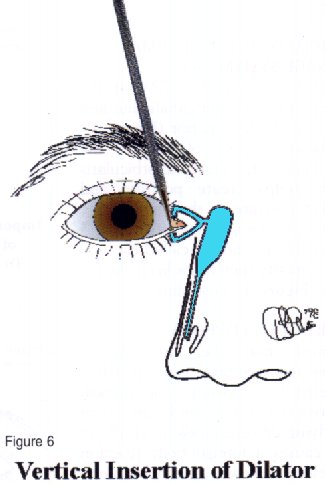
- Insert the dilator vertically
downwards up to 2mm
whilst gently rotating
clockwise and anticlockwise (Figure 6).
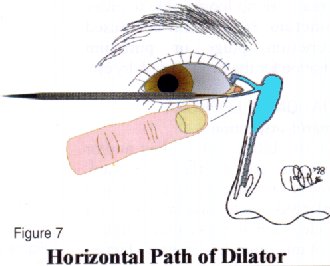
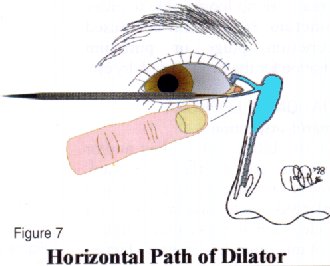
- Pull the lower lid
temporally to straighten
the ampulla and line up
the vertical and horizontal
canaliculi (Figure 7).
- Rotate the dilator
horizontally and insert the
dilator as required.
|
2)Lacrimal syringing
As well as irrigating the
lacrimal system, syringing may
be necessary to dislodge intra-
canalicular punctum plugs.
Procedure
- Wash your hands.
- Some practitioners may wish to put on
surgical gloves.
- Dilate the punctum and canaliculus (see
under 'lacrimal dilation').
- Open the sterile packets of disposable
syringe and cannula and connect them
together.
- Remove the plunger and fill the syringe
with sterile saline.
- Re-insert the plunger, and with the
syringe pointing upward, squeeze out any
remaining air together with some saline.
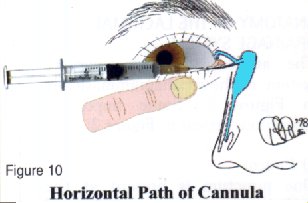
- Insert the cannula into the vertical
canaliculus.
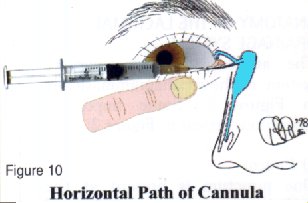
- Pull the lower lid temporally to straighten
the ampulla and line up the horizontal
canaliculus. Rotate the syringe
horizontally whilst inserting until a 'hard'
or 'soft' stop is felt (see over), then pull
back about 2mm (Figure 10).
- Press slowly and gendy on the plunger.
- Ask the patient to report when they
taste saline or feel it in their nose.
|
|
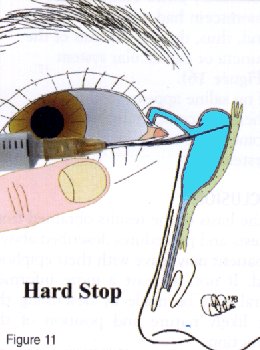
| Hard stop
If the cannula touches the medial
wall of the lacrimal sac and lacrimal
bone, a definite end point is reached.
This is a 'hard stop' (Figure 11) and
indicates that there is no complete
obstruction in the canalicular
system. | 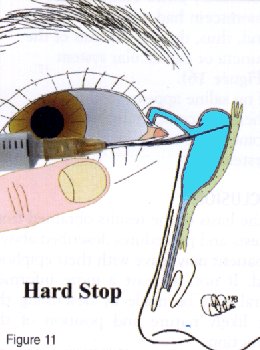 |
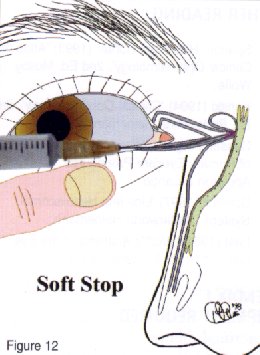
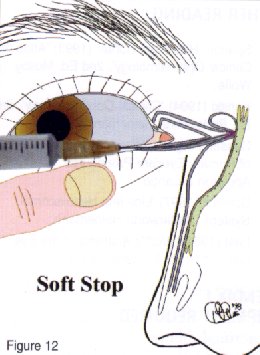
| Soft stop
If a spongy end point is felt, this is
termed a 'soft stop' (Figure 12) and
indicates that the cannula has been
prevented from entering the lacrimal
sac. Therefore, there is a blockage in
the canalicular system and there will
be no distension of the lacrimal sac
when the plunger is pressed.
|  |
Detailed diagnosis
from lacrimal syringing
- If saline refluxes from the inferior
canaliculus, the blockage is there.
- If saline refluxes from the superior
canaliculus, the blockage is in the
common canaliculus.
- If saline passes into the nose, the
problem is hypersecretion of tears or
failure of the lacrimal pump or partial
obstruction of the nasolacrimal system.
- If saline does not reach the nose, there
is a total obstruction of the
nasolacrimal duct and saline may
appear from the superior punctum - the
saline may be purulent if infection is
present - and the lacrimal sac may be
distended.
- An attempt may be made to close the
superior punctum with a dilator or
cotton bud and a further effort made to
clear the obstruction.
|
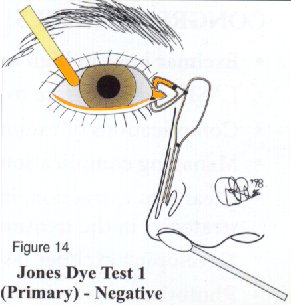
| Functional obstruction
Sometimes, the lacrimal drainage system
may appear patent when syringing proceeds
uneventfully. However, there may be a
functional obstruction. This means that
under the low-pressure circumstances of
normal tear drainage, all or part of the
lacrimal pathway may collapse. Jones dye
tests may be used to distinguish between
patent systems and functionally blocked
ones. | 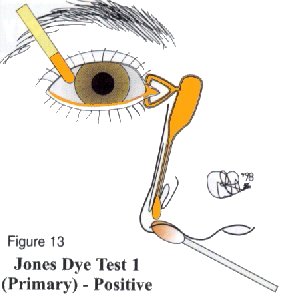 |
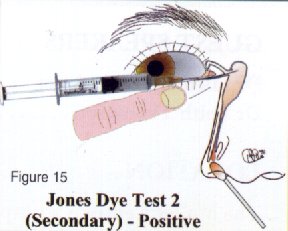
JONES DYE TESTS
PRIMARY AND SECONDARY
Procedure
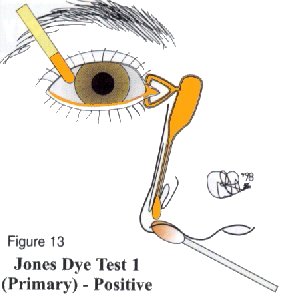
- Instil one drop of fluorescein into the
conjunctival sac (Figure 13).
- Put a cotton bud soaked in anaesthetic
in the inferior meatus.
- If fluorescein is detected after five
minutes, the system is patent (positive
Primary Jones Test).
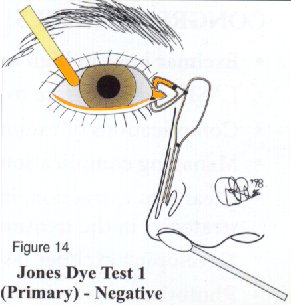
- If no fluorescein is discovered, this
is a negative Primary Jones Test (Figure
14) and the functional obstruction
could be anywhere from the punctum
to the Valve of Hasner.
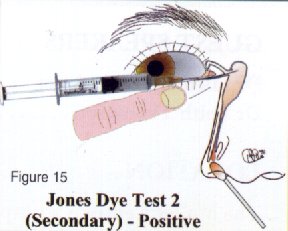
- Next, wash the excess fluorescein from
the conjunctival sac and syringe. If
fluorescein is detected, then this shows
it had entered the sac and constitutes a
positive Secondary Jones Test (Figure
15) and suggests a functional
obstruction of the nasolacrimal duct.
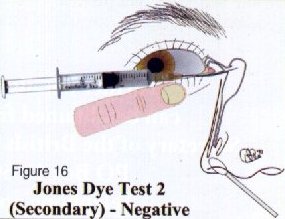
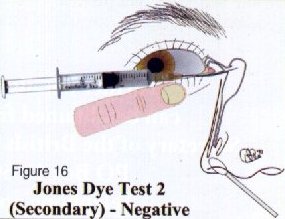
- If no dye is found on the cotton bud
after syringing, this is termed a negative
Secondary Jones Test, because
fluorescein had not entered the sac
and, thus, there is stenosis of the
puncta or canalicular system
(Figure 16).
- If no saline appears in the nose,
there is a complete obstruction
somewhere in the lacrimal drainage
system.
| 
 |
| CONCLUSION
On the basis of the results obtained from
the tests and procedures described above,
the patient may leave with their epiphora
cured. If not, at least a more informed
referral may be made by describing the
most likely nature and position of the
obstruction.
FURTHER READING
- Spalton, Hitchings, Hunter (1993) 'Atlas of
Clinical Ophthalmology'. 2nd Ed, Mosby
Wolfe.
- Kanski (1994) 'Clinical Ophthalmology'. 3rd
Ed, Butterworth Heinemam.
- Casser, Fingerat, Woodcome (1997) 'Atlas
of Primary Eyecare Procedures'. 2nd Ed,
Appleton & Lange.
- Schmidt (1997) 'Lids and Nasolacrimal
System'. Butterworth Heinemann.
- Last (1961) 'WoIft's Anatomy of the Eye
and Orbit'. 5th Ed. Lewis & Co.
APPENDIX I
EQUIPMENT REQUIRED
- Lacrimal dilator
- Disposable lacrimal cannulae
- 3 or 5m1 disposable sterile syringes
- Anaesthetic drops, e.g. Ophthaine
- Tissues
- Aerosol bottles of sterile saline
- Disinfection for the dilators, e.g
- Medi- Swabs
- Surgical gloves?
APPENDIX II
SOME EQUIPMENT SUPPLIERS
John Weiss, 89-90 Alston Drive,
Bradwell Abbey, Milton Keynes
MK13 9HF
Tel: 01908-318017 Fax: 01908-318708
Castroviejo Lacrimal dilator
#0105040 BI 15
Lacrimal cannulae 0108142 7276
Optimed, Alveston House,
11 Broad Street, Pershore
Worcs, WR10 1BB
Tel: 01386-561845 Fax: 01386-555177
Irrigating Lacrimal Cannula
260 Code No.1276
Wilders Lacrimal Dilator 13-071 |
 Typically, in the UK, lacrimal dilation and irrigation are performed in hospital. However, with a little practice and care, it is a relatively simple
procedure for any optometrist or GP to carry out. The equipment required is inexpensive and easily obtained (see Appendices I and II).
This paper will review the relevant anatomy and physiology, discuss the aetiology and evaluation of epiphora (watery eye), and then explain
dilation, syringing and the various dye tests associated with investigating the lacrimal drainage system.
Typically, in the UK, lacrimal dilation and irrigation are performed in hospital. However, with a little practice and care, it is a relatively simple
procedure for any optometrist or GP to carry out. The equipment required is inexpensive and easily obtained (see Appendices I and II).
This paper will review the relevant anatomy and physiology, discuss the aetiology and evaluation of epiphora (watery eye), and then explain
dilation, syringing and the various dye tests associated with investigating the lacrimal drainage system.
 ANATOMY OF THE LACRIMAL
DRAINAGE SYSTEM
ANATOMY OF THE LACRIMAL
DRAINAGE SYSTEM